http://hbswk.hbs.edu/item/3374.html
Monday, July 25, 2011
You have received a shared article
http://hbswk.hbs.edu/item/3374.html
Wednesday, May 11, 2011
The Lean LaunchPad at Stanford – The Final Presentations
Class lectures were over last week, but most teams kept up the mad rush to talk to even more customers and further refine their products. Now they were standing in front of us to give their final presentations. They had all worked hard. Teams spent an average of 50 to 100 hours a week on their companies, interviewed 50+ customers and surveyed hundreds (in some cases thousands) more.
(p.s. they’re going to make a company out of this class project, and they’re hiring engineers.)
- The combination of the Business Model Canvas and the Customer Development process was an extremely efficient template for the students to follow – even more than we expected.
- It drove a hyper-accelerated learning process which led the students to a “information dense” set of conclusions. (Translation: they learned a lot more, in a shorter period of time than in any other entrepreneurship course we’ve ever taught or seen.)
- The process worked for all types of startups – not just web software but from a diverse set of industries – wind turbines, autonomous vehicles and medical devices.
- Insisting that the students keep a weekly blog of their customer development activities gave us insight into their progress in powerful and unexpected ways. (Much more on this in subsequent blog posts.)
- In this first offering of the Lean Launchpad class we let students sign up without being part of a team. In hindsight this wasted at least a week of class time. Next year we’ll have the teams form before class starts. We’ll hold a mixer before the semester starts so students can meet each other and form teams. Then we’ll interview teams for admission to the class.
- Make Market Size estimates (TAM, SAM, addressable) part of Week 2 hypotheses
- Show examples of a multi-sided market (a la Google) in Week 3 or 4 lectures.
- Be more explicit about final deliverables; if you’re a physical product you must show us a costed bill of materials and a prototype. If you’re a web product you need to build it and have customers using it.
- Teach the channel lecture (currently week 5) before the demand creation lecture (currently week 4.)
- Have teams draw the diagram of “customer flow” in week 3 and payment flowsin week 6.
- Have teams draw the diagram of a finance and operations timeline in week 9.
- Find a way to grade team dynamics – so we can really tell who works well together and who doesn’t.
- Video final presentations and post to the web. (We couldn’t get someone in time this year)
Wednesday, April 27, 2011
Cash is king: 8 tips for optimizing your startup financing strategy - Fortune Finance
Cash is king: 8 tips for optimizing your startup financing strategy
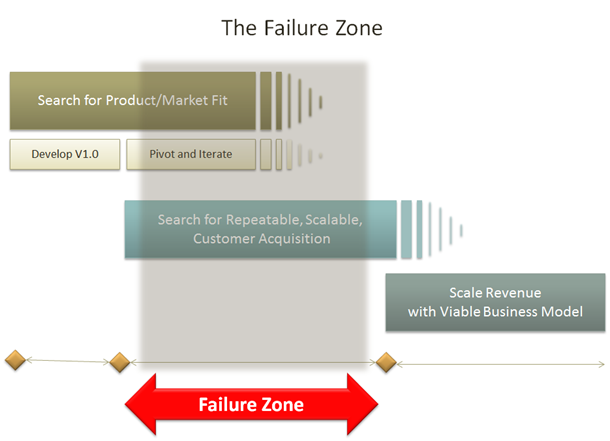
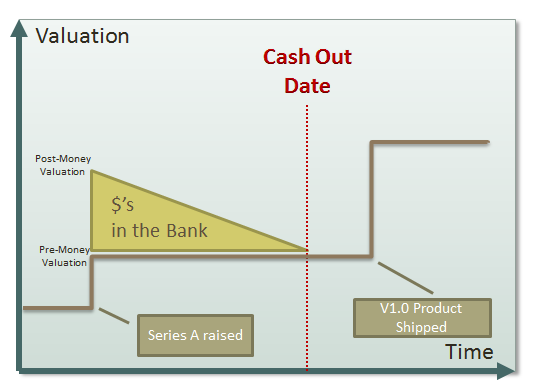
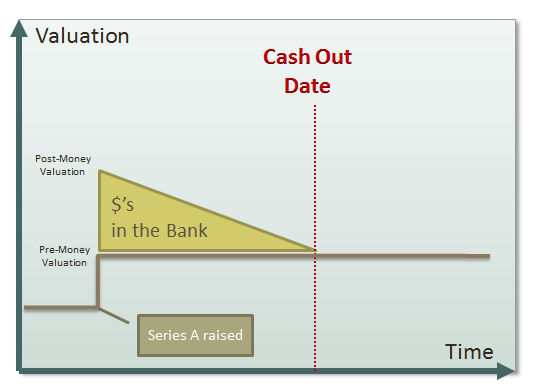
- Make sure that they understand when their cash runs out
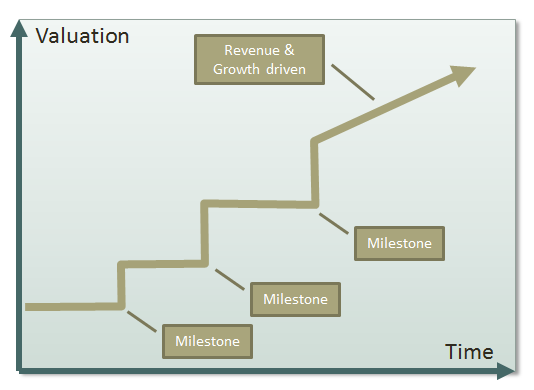
- Understand what milestones have to be achieved to get a higher valuation
- Create the right plan to achieve those milestones in the right timeframe
Usually the single biggest way to show that risk is being reduced is to show evidence of increasing traction with paying customers. If a significant number of customers are willing to pay for a product, that tells an investor many positive things:
- The company has reached product/market fit
- The monetization strategy is working
- The technology works
- The team has shown some ability to execute
- You have shown a wireframe mockup of the application to a significant number of customers and they are willing to talk to investors and tell them that they plan to buy the product when it ships.
- You have shipped a beta of the product to some customers
- Your beta customers are testing the product and reporting success
- You have a large number of free users, and their engagement with the product is high
- You have sold the product to a small number of paying customers
- Your paying customers have put the product into production usage, and are reporting success
- Your customers are coming back and re-ordering, and recommending the product to their friends
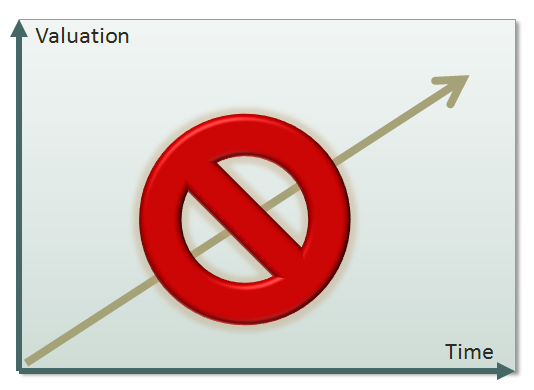
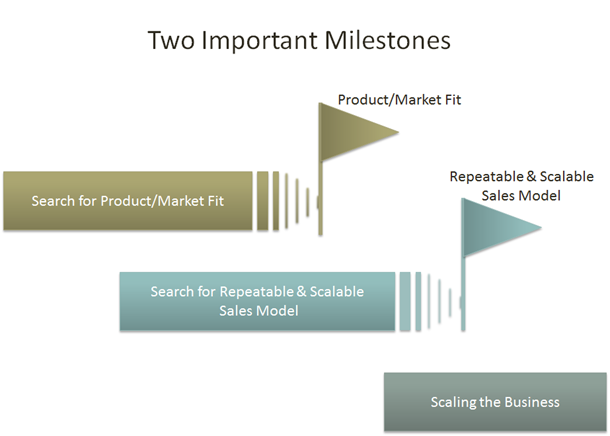
Readers of one of my earlier blog posts, Setting the Startup Accelerator Pedal, will know that I like to think of the lifecycle of a startup in three phases. The first phase is the search for product/market fit. Increasing customer traction is the best way to prove to investors that you have reached product/market fit. The second phase is the search for a repeatable and scalable sales model. Reaching this milestone will greatly increase valuation and attract growth stage investors who like to invest in companies that are ready to scale.
- Hiring a great CEO with a proven track record
- Hiring a strong management team
- Reaching profitability
- Becoming the clear market leader
2. Identify your specific risks
- Team: unproven team. Not clear if they can execute.
- Competitive: crowded marketplace with significant competitors
- Market timing: you're confident about the long term market prospects, but it is not clear when the market will take off.
3. Look for quick ways to litigate risks before fundraising
- The best example of this would be a company looking to raise a Seed or Series A round. Even in this early stage of the business, any proof of customer traction can greatly de-risk your startup and increase valuation. This could be accomplished by sketching wireframes of the application, and showing them to customers. The goal would be to get enough customers to validate that this meets a real need so that they are keen to start using it as soon as it ships, and willing to pay for it. If you were able to walk into an investor meeting with a list of 20 customer that were willing to talk to investors, or had provided you with a written statement to that effect, your chances of getting funded would go up substantially, and your valuation would likely increase.
- In our battery example above, the major risk was technical. A quick way to mitigate the risk (but not totally eliminate it), would be to get the top technical expert in the particular area of science to take a look at the scientific problem you were aiming to solve, and have them render an opinion that this technical approach should work.
4. Either aise enough cash to match the milestones...
5. ... or match your milestones to available cash
- Reduce your burn rate to allow you to complete the milestone before you run out of cash.
- Pick a different intermediate milestone, and ask investors if reaching that will allow you to successfully raise an up-round.
6. Validate your milestone / valuation targets with investors
7. Focus all energies on reaching those milestones
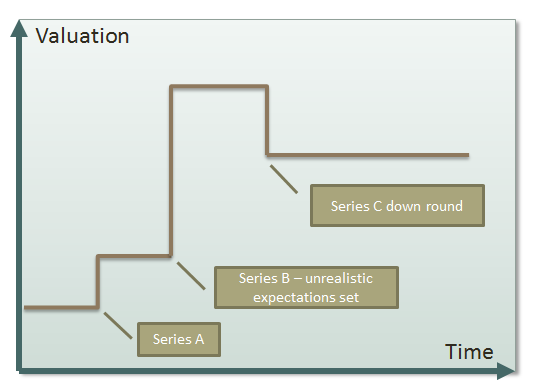
Sometimes down rounds can be caused by raising money at an unrealistic valuation that can't be justified no matter how good the execution. Entrepreneurs who have lived through bubbles understand this well.
Conclusion
My goal was to highlight how startup valuations change based on milestones that significantly de-risk the business. Armed with this information, entrepreneurs should talk to investors to understand how they see the risks and milestones. Then plan and manage their business around achieving desired milestones before hitting their cash out date.
- Take the time to think this through and build a plan.
- Make following the plan a very high priority.
Tuesday, March 8, 2011
Fwd: Forbs: Clayton Christensen: The Survivor, As told to David Whelan 03.14.11, 6:00 PM ET
From: Kwanrat Suanpong <kwanrats@gmail.com>
Date: Tue, Mar 8, 2011 at 3:02 PM
Subject: Forbs: Clayton Christensen: The Survivor, As told to David
Whelan 03.14.11, 6:00 PM ET
To: kwanrats <kwanrats@gmail.com>
On The Cover/Top Stories
Clayton Christensen: The Survivor
As told to David Whelan 03.14.11, 6:00 PM ET
Clayton Christensen, 58, is one of the most influential business
theorists of the last 50 years. The Harvard Business School
professor's 1997 book, The Innovator's Dilemma, introduced in elegant
terms the notion of "disruptive innovation," which explains how
cheaper, simpler or unexpected products and services can bring down
big companies like U.S. Steel, Xerox and Digital Equipment. Every day
business leaders call him or make the pilgrimage to his office in
Boston, Mass. to get advice or thank him for his ideas. A consulting
firm he started popularizes his work, while a hedge fund run by one of
his sons puts money to work betting on disruptive technologies.
One industry that always eluded Christensen's influence was health
care. Caregivers and insurers told him his theories didn't apply to
their complex industry. Christensen knew they were wrong. His
investigation culminated in his 2009 book, The Innovator's
Prescription, written with two doctors. It exposed the many ways
health care was broken and recommended numerous ways it can be
systematized and disrupted the same way mainframes gave way to PCs and
now iPhones.
Christensen's work took on new urgency the past few years as he
suffered a heart attack followed by cancer followed by a stroke. For
Christensen it was not a reason to get too upset. It was another
opportunity, in a lifetime full of them, to gain insight into how to
make the world work better. Because of his July stroke it took a long
time for Christensen to be ready to sit down with FORBES. He was in
intensive speech therapy, eight hours a day at the beginning. But he
graciously agreed to tell his inspiring story in January, the same
month he went back to teaching. Here it is in his words, along with
those of his family, friends and close colleagues.
Clayton Christensen
My dad died at age 49 from Hodgkin's Lymphoma. A wonderful dad. Even
back then in 1975 the probability that it would go into remission was
about 80%. So I happily went off to Oxford. Once I was there for six
weeks it was clear that he was in trouble. The Rhodes Trust was just
marvelous. I went to talk to the warden Sir Edgar Williams and after
two minutes he said, "We'll send you home. You can come back next
week, next month, next year, ten years from now." I was with my dad
for the last two months before he died. It was the most wonderful,
happiest experience of my life to take care of my dad.
He worked for a department store in Salt Lake, ZCMI. As we were
growing up he took us to work on Saturday to help him put the food on
the shelves. I knew his job pretty well. I kept it up [after he got
sick]. That kept us on the same salary and insurance. He dictated to
me his life history. Most I'd heard before. I put it together into a
biography. It's been a wonderful thing. As my kids grew up, on Sunday
morning I'd say, "Okay, guys, read pages 20 to 30 in Grandpa's
biography, and let's talk about what it means for us."
My mom also died of cancer. She was 82. That was just about five years
ago. In the Mormon Church we believe we can be married for all
eternity, not till death do you part. As Mom was getting older she was
excited, truly excited, that within a few years she'd be with Dad
again. I've known people who wanted to die, but most of them were so
miserable they wanted to escape it. But in this case my mom was
healthy. She didn't want to live too long that she couldn't take care
of herself. She was so excited when her doctor said that she had
pancreatic cancer and likely would only live six or seven weeks. She
had a great life and a great family. "Now I can see your dad again,"
she told me.
Ann Christensen (oldest daughter)
My dad is a perpetual student. He'd come home from work every day
excited about some comment a student had made or a paper they had
written. He'd say, "You'll never believe what I learned today." It
turned into dinner table conversation.
Matthew Christensen (oldest son)
Too many of his former students who come back, too many people period,
say family is important or my religious beliefs are important. But if
you look at how they spend any given week, they spend 90 hours at
work. They leave before their kids wake up and come back after they go
to sleep. When my dad was at the Boston Consulting Group, he would go
in superearly and come home early. He was famous for leaving early. We
would play catch in the daylight.
Diabetes
Clayton
I got Type 1 diabetes at 30. It hit me in 1982 when I was a White
House Fellow in Washington. I had viral pneumonia. I lost 35 pounds in
six weeks. And I couldn't see anything. Everything was blurry. I was
always thirsty.
--------------------------------------------------------------------------------
Matthew
One time we visited my mom's sister in Charlottesville. My mom is the
oldest of 12 children, 9 boys. My dad drank a full 2 liters of Seven
Up at dinner. My mom thought that was rude. She was upset. He was
always thirsty.
Clayton
I called a friend who was a doctor in Boston, and he immediately
diagnosed it: "Oh, you have diabetes." I called my wife and said, "Oh,
Christine, I am so relieved I have diabetes. I thought I was going to
die of cancer."
Diabetes is a great example whereby giving the patient the tools you
can manage yourself very well. It's been 28 years. If you have too
much insulin your blood sugar drops and your brain shuts down. I've
only lost consciousness four times in all of those years. The reason
is that I test my blood sugar seven times a day. If it's too low I
have a Snickers bar. If it's high I take a shot. And sometimes I am so
desperate for a Snickers bar I give myself insulin so I can have one.
I figure if I live a normal life I will take about 90,000 shots.
FORBES
The tips of Christensen's very large fingers are covered in black
speckles from the pricks he gives them to test his glucose levels.
These sorts of inexpensive, at-home care devices (Christensen has also
used insulin drug pumps) are the kind of disruptive innovations the
health care system needs to move out of the costly hospital and
medical office setting. Disruption can replace a business that
provides a service with a network that allows people to do it
themselves. You download songs and make your own playlists now instead
of depending on labels to create albums and market them. In medicine
this might mean going from relying on your doctor to keep track of
your diabetes, which he likely has little time to do, to instead
plugging in to a network of other diabetics who can share tips and
provide tools to manage it yourself. Websites like dLife represent
this future. Crohns.org provides tools and facilitates support for
managing that chronic digestive disorder.
Grant Bennett (friend for 32 years)
Overnight Clayton became an insulin-dependent diabetic. He would chart
readings on a sheet of paper. He'd have an upper and lower control
limit, trying to keep as close to the midpoint as possible. My
daughter is an M.D. She says, "The most disappointing part of my job
is people who return to the ER again and again and you tell them what
to do and they don't do it." He's at the extreme opposite. In the
middle of a meeting he would prick himself, test his blood, and then
inject himself in his arm or abdomen.
Matthew
He's a huge, indestructible guy. He's bigger than all the other dads
[at 6 feet 8 inches]. He's had diabetes, but as a consequence of that
he's very careful about what he eats. He would play basketball
Saturday mornings at church.
Ann
When you're in elementary school in public school in our town you have
to write research reports. My siblings and I each did a research
report on diabetes for school.
Heart Attack
FORBES
In November 2007 Christensen had a massive heart attack while the book
The Innovator's Prescription: A Disruptive Solution for Health Care
was in its final stages as a manuscript.
--------------------------------------------------------------------------------
Clayton
It was very strange because there was no evidence of any narrowing of
my arteries. They were wide open. My bad cholesterol level is half the
normal level. And my blood pressure is always on the low side. But a
clot came from somewhere.
For seven years I was one of ten people who have responsibility for
the Mormon Church in the northeast quadrant of North America. Almost
every week I had to go to a city where all of the churches in the area
[known as a "stake"] came together to have a conference. My job was to
help them be better Mormons.
I got assigned to go to Montreal. The stake president in Montreal was
a physician. We stayed at his home. At the meetings on Saturday the
feeling of the spirit of God in that room was deeper than I have ever
felt in my life. It was extraordinary. You walk out of it just
committed to improve your lives for better.
We were sleeping in the extra room in their basement. At about 3
o'clock in the morning I just had a horrible pain in my chest. I never
had a heart attack before. This was something bad. I was thinking, if
I wake Christine and tell her, she'll wake the stake president and
they'll take me to the hospital. It's going to mess up a wonderful
meeting on Sunday. And there are 1,000 members of the church who are
going to come to that meeting. So I knelt down at the side of the bed
and I said to God, "I have a problem. Whatever this is could you
please just make it go away?" And it went away. I fell asleep and the
meetings on Sunday were comparable to the ones on Saturday. The
meetings ended about 9 p.m. on Sunday night, so then we started to
drive back to Boston.
The next day was Veterans Day. I went and raked up the leaves. About 4
p.m. in the afternoon I had a horrible pain. [Christensen still hadn't
told his wife about the episode the night before.] Christine was on
the phone. I grabbed my briefcase because I need to have something to
do when I'm waiting. I said to Christine, "You need to drive me to the
hospital." We started to drive and she said, "What are we going to the
hospital for?" I said, "I think I'm having a heart attack."
She said, "Let me take you to the firehouse, there's an ambulance
there." So we went there and knocked on the door, and she said, "Could
you take my husband into the hospital?" Within about 30 minutes of
when the heart attack occurred we were there.
A clot had come from somewhere and completely blocked the left
anterior artery, which is the major source of blood for the pumping
muscles of the heart. So they sent a catheter up into my heart and
just sucked it out. And as soon as it was gone the flow returned. If
the heart attack happened to me when we were driving home in the
middle of the night or if I'd been on an airplane I would have been
killed.
Dr. Ryan Thompson (Christensen's internist)
It was a major heart attack, the kind that leads to fatalities. It
required immediate stenting. It was the real deal, the so-called
widowmaker. Around a quarter of those who get those don't make it.
Clayton
I told my doctor [about the event in Montreal], and they were so mad
at me. I think God wanted the members of the church to have a great
experience, and he took care of me, too.
--------------------------------------------------------------------------------
Matthew
Our offices were in Harvard Square. I got a call from my mom, who's
crying. She says, "Meet me in the emergency room at Mount Auburn" [a
community teaching hospital affiliated with Harvard]. He had his
briefcase, papers to grade or articles to write. He is horrified about
wasting time. It was a total shock. He had a stress test in June and
had gotten an all clear. And he was supposed to have cataract surgery
that Friday and had a pre-op checkup the Thursday before where he'd
been given an all clear. When your image of your dad is this
indestructible guy, even when you're 30, that's how you think of him.
Seeing him wheeled in on a gurney. It's an image of vulnerability.
Ann
They went in and removed the clot and reinforced the area with a
stent. The doctor came in to debrief us. He got caught a little
off-guard because we [she and two of her brothers] just started
peppering him with questions. We've all been consultants at different
firms, for companies that make those stents. We knew enough at that
point to be relieved. One of the stories that has always been in his
lectures is the impact of angioplasty on cardiothoracic surgeons [how
it disrupted open-heart surgery]. On some level that was comforting,
though we were all still very rattled.
Dr. Jason Hwang (coauthor of the Innovator's Prescription)
With angioplasty you blow up a balloon [in the artery] and it breaks
up a clot. Angioplasty started with balloons that didn't work that
well because the vessel would clamp down. It had a very high failure
rate. But then you added stents to reinforce the vessel, and then
drug-coated stents, and the technology of angioplasty marched upward.
As it gets better it can get more expensive, which opens the door to a
new disrupter.
Matthew
In general I don't think we have big complaints about his care except
for one thing. When he left the hospital he had been put on
medications. When we were waiting to go, for three or four hours, bags
packed, [we] waited for the nutritionist, who never came.
At home my mom had a husband who had just had a heart attack. She was
giving him salads, steamed chard and green leafy vegetables. Those
counteract the effects of Coumadin [a blood-thinning drug]. He went to
his first follow-up, and the INR [a measure of blood thickness] was
supposed to be between two and three. The first reading was a five. We
all have plenty of graduate degrees, but we were fumbling our way
through the dark.
Clayton
The problem from the patient's point of view is that we don't know
what we don't know and therefore we don't ask what otherwise we would
want to ask. When you have handoffs from many to many, as in a
hospital, the probability that things fall through the cracks are just
high. It has nothing to do with how good the individual people are.
Matthew
When he was at Boston Consulting Group [Dad] studied the Michigan
Manufacturing Company. It had nine auto parts plants. One in Pontiac,
Mich. had a mission to make any product for any customer. So you could
run the steel through different types of machines in any sequence. It
had about 20 different sequences and it was expensive. At the other
end of the spectrum was a plant in Maysville, Ohio that just had two
pathways. It could make parts at a very low cost. A hospital is like
the Pontiac plant.
Clayton
As we did the study we realized that every time you double the number
of pathways you raise overhead by 30%. It was not that the Pontiac
plant was badly managed. It just had a different mission. When I
present a diagram of the plants' pathways to a group [with arrows
between machines], I ask: "What if I took the names of the machines
off? Is it still a diagram of an axle plant--or a hospital?" Our
research has found 125 different pathways through a hospital. That's
why 85% of hospital costs are overhead.
FORBES
After his heart attack Christensen bought a home INR meter, which
measures how long it takes for blood to clot, so he could learn how to
manage his Coumadin.
--------------------------------------------------------------------------------
Clayton
The other option is to go down to the hospital. You sit there for 15
minutes, and then they draw the blood out. And they never say, "Sit
here for five more minutes, and we'll tell you the result." Instead
they put it over in the queue. Ultimately they do the sample, and then
the result gets printed out on a sheet of paper. And what happens to
that? Sometimes it goes to my personal doctor, who may or may not see
it, or might see it and not know what initiated this in the first
place. "Should I call the patient, should I go see him or pull him
in?" The data doesn't go to the person who knows exactly what to do
with it. It helped me understand how wonderful and critical it would
be to push care closer and closer to patients and their families.
FORBES
Christensen argues that hospitals should focus primarily on what he
calls intuitive medicine, the process of figuring out what's wrong
with a patient. Once the treatment is set and can be routinized, that
care should be transferred to lower-cost providers. The best way to do
this is to have an integrated system, like what Kaiser Permanente runs
in the western U.S., where the hospital owns the outlying clinics and
surgery centers--and, ideally, also provides insurance. With more
routinized care, nurses can be trained to do doctors' jobs and
specialty facilities can focus on driving out inefficiency with
high-volume surgeries. Better and simpler diagnostics, like a
home-pregnancy test, would allow patients to better care for
themselves. Over time more medical care will follow the path of
treating infectious diseases, which in the past might have required
hospitalization but now can be treated with a prescription from a
nurse.
Clayton
If my INR is above three the result is Christine makes kale soup,
which makes your blood clot much faster. If it's low then we don't
have those kind of green vegetables. On-the-spot care works if you do
the test yourself, because that information causes you to do something
different.
Ann
After the heart attack Dad went through a very careful, deliberate
process with all of us and his assistant, thinking about all the
things he was involved with and where he could cut back. He definitely
wasn't able to travel as much. But that let him be at home in Boston.
He was able to work on the health care and education books. You want
to say he was stressed and if he's less stressed it won't happen
again. He works hard, but he's not a stressed-out guy. There's a
difference.
Grant
Clayton works very, very hard. As his consulting career took off he
traveled a great deal. He was always a very dedicated husband and
father. But over the years we'd have conversations about the
fundamental lifestyle questions. When Clayton had the heart attack,
the thought running through my mind is that this may be the one event
that may cause Clayton to slow down and not travel as much.
Cancer
Clayton
I was in Washington [in December 2009] with Christine. The church has
a temple there on the Beltway, and at Christmastime they have jillions
of lights decorating the gardens. We got invited to come down for the
ceremony. That night we stayed near Reagan Airport, and at about two
in the morning I had this awful pain in my lower back. I tried all
kinds of different positions. Nothing seemed to help. At three I went
down to a 7-Eleven. I got a bunch of ibuprofen. That didn't work. When
I was a high school senior I had an infection in my kidneys. And this
thing felt exactly like that felt. So we came home on the first plane.
I went immediately to a MinuteClinic. I thought, "I'll just get a
urine test." It turns out in Massachusetts that MinuteClinics can't do
that. We had to go to Mount Auburn Hospital, the same place we took
care of my heart attack.
FORBES
Christensen has advocated for the retail clinic concept, where care is
delivered in the back of a CVS or Walgreens. There's a menu of
conditions on the wall, like pink eye and poison ivy, and a simple
treatment protocol for each. Why shouldn't nurse practitioners and
other professionals like pharmacists, optometrists and
nurse-anesthetists be given more responsibility? They can deliver care
more cheaply than doctors.
Clayton
[The hospital] did the test. There was nothing that suggested
infection. The head of the emergency is the same guy who orchestrated
the care of my heart attack. He started to feel my side. And
basically, without telling me, he thought there was something big
inside of me. He thought it was my aorta that had ballooned up. They
very quickly did an ultrasound. They were all ready to cut me open and
deal with an aneurysm. But the ultrasound showed that it wasn't an
aneurysm. He said, "I have some good news and some bad news. The good
news is you don't have an aneurysm. But you do have really big masses
in there that feel forever like tumors." So he said, "I'm sorry." He
was very kind.
FORBES
After consulting with Dr. Thompson and another physician friend,
Christensen transferred to Massachusetts General, a Harvard-affiliated
teaching hospital downtown. An oncologist met with Christensen that
afternoon.
--------------------------------------------------------------------------------
Clayton
The tumor in my abdomen was the size of a ball this big [mimes a
football]. It was pushing against my back, and that's what I felt.
There was another one behind my sternum that was wrapped around my
esophagus and it hadn't yet started to squeeze things down, but it was
poised to do that. The third one was behind my clavicle. It was about
the size of a jewelry box. That's the one they biopsied.
Matthew
Ephraim Hochberg, he's the oncologist who oversaw all of my dad's
care, could not have been better. Hochberg told us, "From what you
described, let me tell you what it is." I remember the percentages
added up to 110%--70% lymphoma, with three different types; 20% lung
cancer. The others were, I think, sarcoma and small-cell cancer, or
testicular cancer. Metastatic lung cancer was the worst-case scenario.
Clayton
They started doing all these tests. But this time I think I was more
knowledgeable because The Innovator's Prescription had been out, and a
big theme of that is that the body has a limited vocabulary to draw
upon to express that there's a disease inside. There are many more
diseases than symptoms. There are over 50 types of lymphoma. Dr.
Hochberg, I love to listen to him. He describes how lymphoma respects
the boundaries [of the lymphatic system]. It would rarely do something
so rude as to invade another organ, which was great news for me. The
lymph system is comprised of all of these tiny little tubes throughout
my body that collect stuff. Now all of a sudden you have three big
masses, but they were within the system that controlled them.
Dr. Ephraim Hochberg (clayton's lymphoma specialist)
Ninety percent of people will have microscopic evidence of lymphoma in
their blood--90% of people. The question is why 99% of those people
never get lymphoma. I got a phone call from [Christensen's] primary
care physician asking if I could see a patient. When I went to meet
him it was in the surgical waiting room. He was being prepped for a
biopsy. He was, even at that point, remarkably composed and
well-spoken. Especially with the lack of knowledge of what kind of
cancer this was. Everyone was extremely calm. I don't know how much of
that calm and reserve stemmed from his personal faith and how much
stemmed from his faith in our hospital, but I suspect that much more
of it was the former than the latter.
FORBES
After the biopsy Christensen received a diagnosis of follicular
lymphoma. It looked like a slower-growing variety, which would be less
responsive to chemotherapy and more likely to be terminal.
Clayton
I thought about it. I knelt down and made a commitment to God: "I
think I probably have done things in my life that you wanted me to do.
And if in your judgment there's more work that needs to be done on the
other side, I'm happy to go. And on the other hand, if I can be more
useful by staying in this side my preference is to stay. I don't want
to leave my kids and Christine just yet." I felt good. I don't think
that it was in any way depressing. In God's interaction with Adam he
didn't in any way promise that it was going to be easy. Even if you do
the right thing, there's a lot more that you need to learn--and a lot
of learning comes from adversity.
Dr. Hochberg
[After some more testing] it turned out he had a variant of lymphoma
that we described in a research paper five years ago. The cells look
small, but the rate at which they divide as measured by another test
is quite high. So there's a potential that some might even be cured
with a more aggressive type of chemotherapy. So we went from "It's
incurable" to a rare subtype of common lymphoma.
Clayton
As a complete, independent event, when I showed up at Mass General and
they were doing a workup, I just made this observation. In my right
eye there is this curtain that comes across, and it's all gray. My
retina was detached. Right there is the Mass Eye & Ear infirmary. They
decided that I probably ought to get the retina re-attached before I
started the chemo.
It was just fantastic to see the technology. The laser is like a spot
welder. You can hear it. [He makes two gunshot sounds.] It creates
scar tissue that tacks it to the back of the eye. They suck out the
vitreous [jelly] from your eye and replace it with silicone oil. The
silicone molecules are huge. They're too big to go through these
little pinholes in the retina [and cause another detachment]. When you
look out through these massive molecules everything is fuzzy for a
while. But, holy cow, how can I complain when this is saving my
eyesight? Who are the guys who developed the silicone gel that's so
pure? Who's the first guy who had the guts to open up the eye and
stick this laser in and go bing?
--------------------------------------------------------------------------------
FORBES
The surgeon who performed the procedure, a vitrectomy and laser
retinopexy, would have needed ten years of training to operate inside
the eye. These procedures should and will become commoditized. Lasik
surgery is retailed directly to patients and not covered by insurance.
Its price has dropped dramatically since its inception in 1995. In
Singapore technicians have supplanted doctors in reading annual
diabetic retina scans. A similar disruption, in dentistry, is the
Invisalign mouthpiece, which straightens teeth without orthodontics.
Prior to Christmas Dr. Hochberg prescribed a cocktail of chemotherapy
drugs plus Rituxan, a targeted antibody from Genentech. Christensen
began getting infusions every three weeks for four and a half months.
That spring semester he continued working, speaking and doing some
teaching on a reduced schedule.
Clayton
Dr. Hochberg wanted me to stay in the saddle as much as I could
because that keeps you from thinking about yourself. You go down and
hit bottom about seven days after the therapy, and then by ten days
after you feel great. When my father was suffering from a very similar
disease, after he had one of his rounds I went in and just sat by him
and said, "Dad, how are you doing?" And he said, "I had no idea how
sick you have to be in order to die." Chemo is a lot easier to
tolerate now.
FORBES
After the first two rounds of chemotherapy, Christensen had several
scans to see how the tumors had responded.
Dr. Hochberg
He had a dramatic response. His first scan he had a mass in his
abdomen of 14cm by 8cm. On the second scan it was down to 8cm by
6cm--so, volumetrically, about a 75% response. The last scan we did
showed the mass was down to 4cm by 3cm.
Clayton
It was actually really fun to see Dr. Hochberg. He let me in the
office, excited about what he was learning. He truly was energized to
teach it to me. He's a true scientist. So he would never exaggerate.
He showed me the data in such a very excited tone of voice. Before
Rituxan came along, you could say probabilistically for the population
that you're going to be in remission for 4.3 years. If you keep taking
Rituxan for maintenance, you've expanded the probability of it staying
in remission out to 7 or 8 years. Dr. Hochberg raises the possibility
that in my case it won't come back. As he looks at what's happening to
my particular tumors, they just seem to be disintegrated. But you
never know. If it doesn't ever come back, then you know you've been
cured. That's all you can really say at this point.
Dr. Thompson
The most striking thing with Clayton was when I once visited him in
the chemo unit. He's sitting there receiving the infusion that makes
you feel miserable. But he just wanted to talk about my family. It
made me feel like a million bucks. Most people would want to just
sleep. His hair came out, and he had some neuropathy, some nerve
damage to his feet. By and large he did well.
Clayton
One day before chemotherapy, I woke up in the morning and went
downstairs. There on the kitchen table was this framed photo that had
Matthew, Mike [my second son], Spencer [my third son] and then Matt's
little boy named Clay [who is two years old]. They all had shaved
their heads to show solidarity and took a picture. They framed it with
their locks of hair under the glass. It was very sweet.
FORBES
Christensen moved on to lighter-maintenance doses every two months.
These will continue for two years. Hochberg estimates that
Christensen's total cancer care might cost $150,000 or $200,000.
Rituxan costs $8,000 or $10,000 a dose, just by itself.
--------------------------------------------------------------------------------
Dr. Hochberg
Academic medicine is an expensive way to provide therapy. When he
needed integrated therapy with his retinal detachment and his
lymphoma, he could have a world-class retina doctor seeing him at the
same time.
We're beginning to take cancers and classify them into "This is a
particular genetic subtype, let's treat it this way," versus "This is
a complicated disease; we don't have good therapy; stay with the
diagnostic shop."
In an ideal world Clay's system would have folks coming through a few
diagnostic shops like a big cancer center. Then they'd find a great
doc near them who can provide their care efficiently in the community
with a plan that's set in place. I also remember a discussion in the
beginning with Clayton about the transportability of medical records
and whether or not a universal medical record of some type would have
allowed some simplification. We ended up doing a lot of repeat blood
work because the records of the Boston hospitals aren't contained in a
single place.
Stroke
FORBES
Christensen had been out of chemotherapy for three months. But on July
18, 2010, while giving a talk at 6:30 in the morning on a Sunday to a
church group, he suffered a stroke.
Matthew
The stroke was the most distressing. I was at the church meeting. And
one of the things that my dad loves to talk about in our church
meetings is how to share the Gospel with other people. Midsentence he
couldn't talk. It was nonsense. I tried to help him sit down and put
my hands around his arms. His face looked fine. We thought: "Gee, this
might be a low blood sugar thing." He keeps candy in his briefcase.
I'm feeding him Skittles and Snickers. After about ten minutes he was
not getting better. We tested his blood sugar. It was 325 [not low].
We went out in the hall. My friend Mike Preece [a neuroradiologist]
came out with us and gave him a neurological exam. He held Dad's hands
with his fingers and said, "Can you squeeze my hands?" He said, "Yes,"
but he couldn't do anything. I could tell just from Mike's body
language and the other doctors there [at the meeting], this is a
dead-serious situation. By the time we got to the hospital he couldn't
walk. I remember pushing him in a wheelchair, putting his briefcase in
his lap.
For someone that's always had the image most kids have of their dad
being Superman, and him having always been such an articulate person,
it was hard. You try to talk to him and he would say things and they
made no sense. I was thinking, "What's going to happen? Will he be
okay or not?" I think he's done so much and done so much good. What
else is there for him to do? The end comes for everyone. And could it
be for him?
FORBES
At Mass General Christensen, within an hour, received a clot-busting
drug called TPA, which has been shown to help minimize stroke
complications.
Dr. Thompson
There's nothing that unifies what happened to Clayton. Each is not
that uncommon. Stroke is the third-leading cause of death, heart
attack is number one, cancer is number two. But the chances that one
person would have all three is uncommon. Type I diabetes is a risk
factor for heart attack and stroke. But there's nothing unifying all
three.
--------------------------------------------------------------------------------
FORBES
The stroke managed to avoid the part of his brain that controlled his
motor skills and analytical abilities. He did, however, lose his
speech. In a recent lecture to HBS students, he described the
sensation by comparing it to a file cabinet in his head filled with
words--that is suddenly tipped over.
Christensen's inability to speak and write had the potential to affect
many of his projects. His consulting firm, InnoSight, now employs 60
people. At Harvard Business School he had just launched a project
called the Forum for Innovation & Growth, which tapped hundreds of HBS
grads and executives to help generate and proliferate new management
theories. And he had created a think tank to tackle public policy
issues--especially health and education.
Grant
Two weeks after the stroke we went out to dinner together. We went to
the Charles Hotel restaurant Henrietta's Table and met a couple of
other friends there. We said, "Clayton, tell us exactly what
happened." [He said,] "I'm at this church meeting and I feel dizzy.
And before I know it I'm at that . . . What's that place where the
doctors get together?" And Christine said, "A hospital." "They had
tests. I had--what was the condition?" "It was a stroke, Clayton, it
was a stroke."
Clearly gone were certain vocabulary words. We were talking about the
Fed and interest rates. And not one shred of his basic intelligence
was gone. It was simply that certain words weren't there. Now, though,
if you have a conversation with him, you'll have no clue [of his
illness].
Ann
He'd call the hospital for rehab therapy or speech therapy, and they'd
say, "Our first appointment is three weeks from now." To be fair to
those doctors, they're full. Even in the hospital, within a couple
days of the stroke, he wanted to start practicing. He'd make lists of
words on a topic.
Stephen Kaufman (former CEO of Arrow Electronics, current Harvard
Business School professor)
All three of his problems [heart attack, cancer, stroke] were on the
severe side, needing the big hospital with the big tools. But the
recovery from his stroke would be representative of what can be
routinized. There's a large body of knowledge that can be used in the
therapy. It doesn't have to be done at Mass General.
Matthew
While he was waiting for speech therapy he went and bought Rosetta
Stone English. There's an image of something on the software and you
say the word. He'd have contests with my oldest daughter, Madeleine [6
years old]. He lost a lot.
Clayton
I'm an optimistic person. But for the first time in my life, with all
my problems, I focused more and more on me--and it was depressing,
literally. Sometimes I just wanted to quit trying to learn and speak
and write again and just go into my basement and build furniture. I
learned an important lesson from this. I learned that focusing on my
own problems does not bring happiness. God didn't say, "Okay. For
those with problems it's okay to focus on yourself. And for those who
don't have problems, I want you to focus on helping others." Even in
dire times God does not exempt me from his commandment to focus my
life on others, because it transforms hardship to joy.
Matthew
In the vein of kicking a man while he's down, chemo knocks out the
salivary [gland], which knocks out your calcium on your teeth. So now
he has to get implants in all four quadrants of his mouth. His
dentist, who has been wonderful, accommodated him with seven-hour
marathon sessions that include some jawbone reconstruction.
--------------------------------------------------------------------------------
Matthew Eyring (president of Innosight, Christensen's consulting firm)
He talked to a presidential candidate or two. He's spoken to some
members of Congress and senior members of the Administration. What is
tough for him is that his insights into the health care system and
what needs to be done are truly breakthroughs--and they really work.
His disappointment is that it moves very slowly.
Clayton
I've had those meetings, but I'm unable to help Mitt Romney or Nancy
Pelosi and everybody in between. I think [my] brain is really good at
getting through the complexity. I'm not nearly as good at distilling
it into soundbites.
Dr. Hwang
The two doctors who co-wrote our book were both Democrats. Clay has
been adamant that the Obama legislation creates more problems than it
solves. Health care is very innovative in ways that we would call
sustaining. We are careful to explain that the U.S. system is the best
in the world. You'll get superior treatment. But for marginal
improvements in care you're adding tremendous costs. The concern is in
overshooting. To take care of people you need systems that are
lower-cost. We need to free up beds, free up doctors and empower
nurses.
Clayton
There's an interesting observation, I think, that would stand up to a
Ph.D. dissertation, but nobody's done it yet. Sustaining innovations
[those that add to or improve a product already in existence as
opposed to truly disruptive ones] drive inflation up at 6% to 10% a
year. So if you're working for Medtronic and you're in new-product
development, the thought process is: "We need a new product that we
can sell for higher prices and better profits to our best customers."
This isn't wrong, it's just the way the world works. At Harvard--you
look at the opulent facilities that are available to our students
compared with what it was 30 years ago. We have to keep ratcheting up
our facilities and our cafeterias. Our classrooms have padded chairs
and carpet, because if we don't keep providing more we can't compete
with Stanford. All these things drive prices up. What drives prices
down is disruptive innovation.
In health care there isn't anybody who has the scope to change
everything at once. The insurance company can work on processing paper
better. The hospital can try to improve its utilization of its
operating suites. It can try to use its MRIs better. Everybody can
optimize their piece of the system, but they can't rethink everything
in a systemic way.
What I hope is that my material can go to Washington as nonpartisan,
as just a foundation of understanding. If they have the same way to
frame the problem, then the Republicans and the Democrats should be
able to work together much better. The Americans look at Canada,
Europe and Australia, where the government is the payer. Maybe we
ought to adopt their model. And the Europeans and the Australians are
saying, "You know, this isn't working very well, maybe we ought to
adopt the U.S. model." That's the wrong categorization scheme. The
right one question is "Should we be integrated (like Kaiser Permanente
or Finland), or should we be modular (like Partners in Boston and the
Canadian and German systems)?" It's not public versus private.
Ann
I'm not sure how to describe how shocking it's been to have this
happen one after another. He is acutely aware of how lucky he is, and
I think knowing that it could have been worse has been a helpful
perspective. He's not the kind of guy who feels sorry for himself.
It's a blessing that he's alive and treatable. Our family is very
close. We've all leaned on each other a lot.
Matthew
Superficially you could say it's unfair that a guy who has worked so
hard to be healthy could be slapped with a heart attack followed by
cancer followed by a stroke. We believe there's a reason for it. But
we don't understand all of it. As this started to happen, a flood of
everything from cheerful telephone conversations to Facebook wall
posts talked about how inspiring my dad has been to them. It was
pretty humbling.
At one point in the middle of this, we were thinking of getting a
second opinion. I networked into a guy at Mayo. He was familiar with
my dad's research. He said, "Your dad has changed my life. Anything I
can do, I'll do." A lot of people when they go through near-death
experiences look at their lives and feel like they have to make big
changes. My parents in fact have not made big changes. They feel like
they're living the way they should.
--------------------------------------------------------------------------------
Clayton
When I was at Oxford, each one of us had responsibility for three or
four families in our congregation, which we call a ward. Another
student at the university and I were assigned to look after quite a
poor family. I learned that their 10-month-old baby, Wendy, had been
in the hospital for six months. She couldn't digest anything. Wendy
had the body of a newborn, but her face looked like a 10-month-old's.
They had decided nothing could be done. So my companion and I said
let's go see Wendy, and we went there and understood the situation. I
then had a feeling in my heart, which I feel came from the Holy Ghost,
that in this case God wasn't trying to bring her home. Wendy was
sleeping. So we put our hands on her head, and through the power of
God and authority of the priesthood, blessed her. And she got better.
I don't view it as mystic. I believe that God is our father. He
created us. He is powerful because he knows everything. Therefore
everything I learn that is true makes me more like my father in
heaven. When science seems to contradict religion, then one, the
other, or both are wrong, or incomplete. Truth is not incompatible
with itself. When I benefit from science it's actually not correct for
me to say it resulted from science and not from God. They work in
concert.
Dr. Christensen Is In
Disruption is the cure for what ails health care.
Since the late 1990s Christensen has been influencing change in health
care through both his summer leadership program at Harvard Medical
School for hospital administrators and regular consulting work for
medical giants like Johnson & Johnson and Medtronic. Recently he
helped J&J develop a device that would make it easier and cheaper to
administer anesthesia. (The Food & Drug Administration rejected it.)
His book The Innovator's Prescription (2009) was co-written with two
doctors, the late Jerome Grossman, who ran Tufts Medical Center for 16
years, and Jason Hwang, a former student of Christensen's. Hwang
contributed enormously to this story.
The authors acknowledge that the fee-for-service reimbursement system,
in which providers earn more by treating patients more aggressively,
impedes the kind of disruptive innovation that would lead to better
care at a lower cost. There are several systems we could adopt that
would be better, but there isn't a road map to get there. The business
models of health are frozen in the hospital and the doctor's office.
The path to fixing the system is to disrupt those models. Here are
some approaches:
Routinization. A hospital is really three business models under one
roof, each of which manages a different type of medical practice.
Intuitive medicine is the realm of highly trained specialists handling
difficult diagnoses and treatment. Empirical medicine is the costly
realm of chronic care and trial-and-error treatment. Precision
medicine, the real goal for the system, is a case where diagnosis is
known and so is the therapy. Then treatment can be routinized and
moved off-site. Disruption will involve pushing more of medicine into
the precision category, then automating that care to make it better
and cheaper.
Consolidation. The best way to unleash disruption is if more health
care providers combine, controlling hospitals, doctors and health
insurance. Christensen makes an analogy to RCA in the 1950s. To get
people to watch the first color programming on its NBC channel, RCA
also had to manufacture color TV sets. A hospital loses money if it
tells patients to go to an outside cheaper clinic. But if it owns the
health plan and the clinic, disruptive ideas will flourish.
Precision. The kind of targeted therapies now used in cancer
treatment, such as the drug Christensen received, will be applied more
widely. Diseases will be subtyped more specifically and therapies
tailored to work better. This will also save time and money as
clinical drug trials become more focused. Specialty clinics will arise
to implant devices more cheaply.
Do-it-yourself. Christensen predicts a rise in self-diagnosis and
self-care, as tools that used to be stuck in the hospital reach
patients and their families.